Vaccine Booster
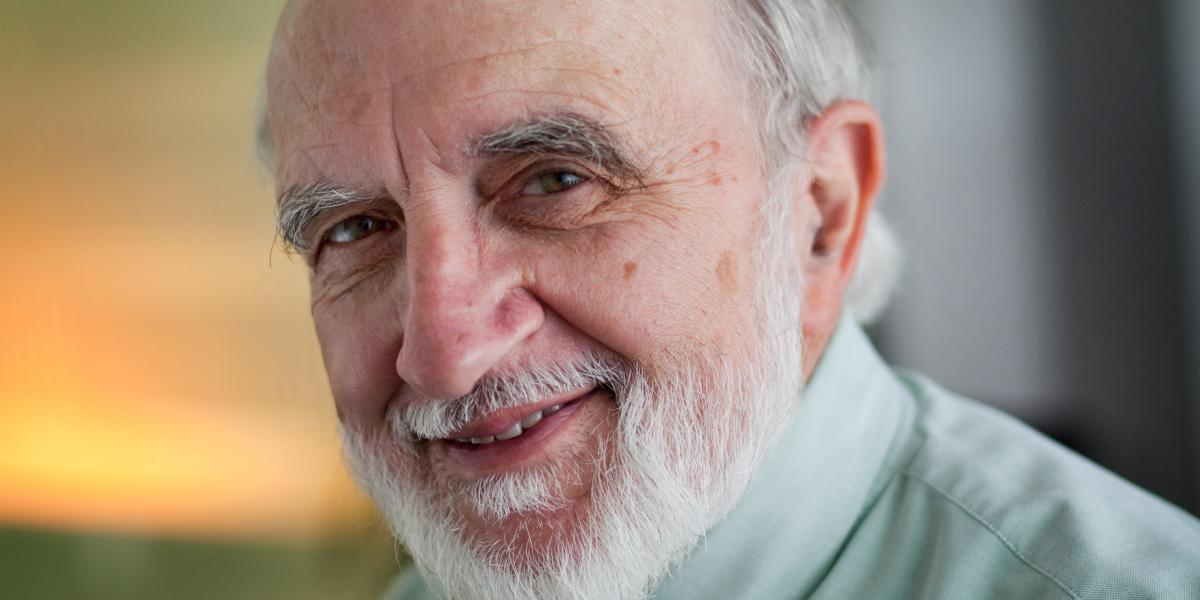
Measles cases in the U.S. hit a 15-year high this year. Pertussis (whooping cough) resurged in the U.S. last year, especially in California where there were 9,100 cases and 10 deaths. These and other outbreaks are related to parents withholding recommended vaccines and obtaining exemptions for their children from childhood immunizations required for attendance at schools, says Neal Halsey, MD, director of the Bloomberg School’s Institute for Vaccine Safety. Halsey has forged his convictions about vaccine safety and effectiveness through 40 years of rigorous evidence reviews and personal observation. In 1971, he witnessed measles tear through the pediatric ward of a Nicaraguan hospital, infecting young patients and killing two children. “That was an eye-opener to me about how severe this disease could be,” says Halsey, now an International Health professor. In a summer interview with Brian W. Simpson, editor of Johns Hopkins Public Health, Halsey reflected on the persistence of vaccine-preventable diseases, parents concerned about vaccine risks, new vaccines and the difference between vaccination and immunization.
Are recent pertussis and measles outbreaks in the U.S isolated cases or is the system failing?
We have high immunization rates in this country; well over 90 percent of children have received the recommended vaccines—over 95 percent by the time they enter school. But the system isn’t perfect, and the system isn’t getting children immunized as timely as they should. And with delays in immunization, you have enough susceptible children that can accumulate that you get disease outbreaks.
Can high rates of exemptions actually endanger children who have been immunized?
Yes. The vaccines are not perfect and so not everybody who gets vaccinated gets full protection against the disease. And so some remain susceptible. More importantly, there are children who have true medical contraindications to getting vaccinated. Children who have diseases [like leukemia] can’t get the live vaccines like measles, but we need to protect those children by immunizing everybody else. And those children should be allowed to go to school—and to go to school without fear of getting exposed to a disease that could kill them.
Are most cases of measles today in the U.S. homegrown or imported?
We do not have continued transmission of measles in the U.S. But we get these repeated introductions from travelers. And that’s going to continue until measles is eliminated everywhere.
When you look back over your career in vaccines, what’s most surprised you?
I think the thing that has most surprised me—and it’s a pleasant surprise—is the introduction of new vaccines like the hepatitis B vaccine and universal use vaccines against Haemophilus influenzae, pneumococcal disease and rotavirus. When I was an intern, I spent more than half the time taking care of children with meningitis from Haemophilus influenzae or pneumococcus. And now those diseases are largely disappearing due to the introduction of those two vaccines.
Does it frustrate you when people avoid such vaccines for their children?
Yes. It is very frustrating to hear people perpetuate myths and misunderstandings about vaccines. And I can tell you from having talked to a few parents of children who have developed these diseases that, to a person, they said, “We had no idea it could be this bad.” That influenza could lead to death, which does occur. Or that not getting a vaccine could result in severe disease. I saw that repeatedly with measles. Many parents today think pertussis is a disease of the past, but it’s not true. It’s here.
“I can tell you from having talked to a few parents of children who have developed these diseases that, to a person, they said, ‘We had no idea it could be this bad.’”
What’s the best way to reach parents who have genuine concerns about vaccines?
If they raise questions, we have to talk about those. It’s our job to help separate the fact from fiction. We need to have our public health authorities and physicians armed with the information to show parents what’s true and what’s not true. And they need to be aware of the potential severe complications that are prevented by these vaccines. That’s what’s missing from the experience of most young parents. They don’t see children with measles or severe pertussis.
How would you rate the public health efforts thus far?
I think we’re doing a very good job in this country, but it’s not perfect and it would be nice if all children who were eligible to receive vaccines did receive them and receive them on the recommended schedule. But the reality is, there are some delays and there are some refusers. But we need to stick with those people and to help them through the process. Some will change their mind. Some won’t.
If you could change one thing about the vaccination system in the U.S., what would you change?
We should have a policy of universal immunization, but the high cost of some vaccines—like the HPV vaccine—is a barrier to the optimal policy of immunizing males as well as females. So if I could change anything, it would be to empower public health authorities to engage the manufacturers in discussions about vaccine prices to help make optimal vaccine policies highly cost effective. In Canada they have the ability to negotiate like this. [In the U.S.,] we’ve got strict rules that prohibit that kind of a thing.
What new vaccines are in the pipeline?
There are a number of vaccines in development that have promise for being licensed and used on a widespread basis. Here at Hopkins, Anna Durbin is working on vaccines to protect against dengue infections. Ruth Karron is doing studies on [vaccines for] respiratory syncytial virus, a major cause of respiratory disease in children. We have the potential for other vaccines to protect against diseases such as group A streptococcal infections, staphylococcal infections, malaria, and perhaps HIV. There is the potential for other vaccines to protect against cancer. I wouldn’t say that those are likely to be licensed within the near future. There is also the potential for vaccines to protect against autoimmune diseases like multiple sclerosis and rheumatoid arthritis.
Is there a difference between “vaccination” and “immunization?”
Yes. The terms are used interchangeably by many people, and that’s probably okay. Technically, vaccination is administering a vaccine. Immunization is the process of administering a vaccine that results in an immune response that’s protective.
Therefore, an immunization is a successful vaccination.
That would be one way to put it.